Since the pandemic began, any patient with symptoms that could signal covid-19, including coughs, respiratory symptoms, fever or loss of taste or smell, must be kept separate from all other patients, and seen in ‘hot’ areas of hospitals only. To prevent possible covid-19 patients entering hospitals, a lot of testing is now done in drive-throughs. Monitoring of these patients is more likely to be done remotely.
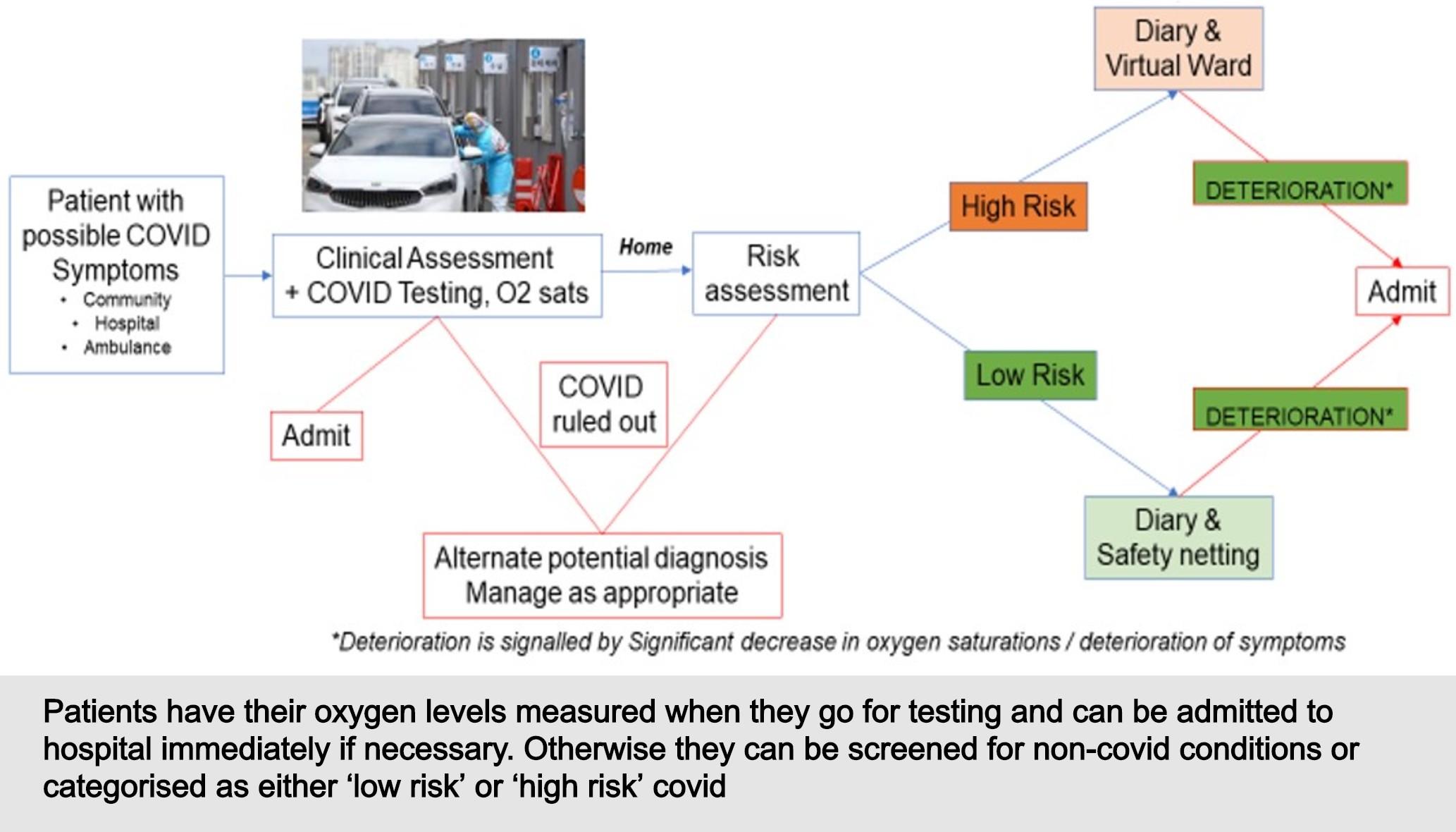
We are proposing where patients are tested by a healthcare professional rather than self-testing that patients’ oxygen levels be measured at the same time as they are tested. This will enable patients who are already experiencing silent hypoxia to be identified promptly and be admitted to hospital at an early stage. The earlier they are treated, the better their outcomes will be.
However, most patients will return home after testing, although they will be safeguarded.
At this point, suspected covid patients are defined either as ‘high risk’ (including older people, patients with co-morbidities, those with black, Asian or minority ethnic (BAME) status or those on high-dose immunosuppression), or ‘lower risk’ (such as younger patients). They are then managed in a ‘virtual ward’ as shown below, with the lower risk patients keeping a diary of their symptom severity and instructions to call NHS111 if their symptoms worsen. NHS England has produced a leaflet for patients with suspected coronavirus to help them self monitor for symptom progression. This guidance also helps patients calculate whether they need to contact NHS111, or call an ambulance.
Higher risk patients also keep a diary and monitor their oxygen levels with a pulse oximeter. But when they enter the virtual ward they have more contact with healthcare practitioners through telemedicine — either video or telephone calls with their GP or nurse. This means they have closer monitoring and can be treated promptly or admitted to hospital quickly if necessary.